Pharmaceutical Quality Assurance -Drug and Therapeutics Committee Training Course
CONTENTS
Pharmaceutical Quality Assurance
Acknowledgment
Purpose and Content
Objectives
Outline
Key Definitions
Introduction
Determinants or Aspects of Medicine Quality
Critical Elements of a Comprehensive Quality Assurance Program
How Is Quality Assessed?
How Is Quality Assured?
Who Ensures Medicine Quality?
Pharmaceutical Quality Assurance—Implications for the DTC
Providing Technical Advice on Procurement of Pharmaceuticals
Providing Technical Advice to Other Departments
Analyzing Product Problem Reports
Activity 1. Quality Assurance Issues and Concerns
Summary
Acknowledgment
Material in session 5 is adapted from Management Sciences for Health’s Managing Drug Supply, chapter 18, “Quality Assurance for Drug Procurement” (MSH 1997).
Purpose and Content
The purpose of quality assurance (QA) in public pharmaceutical supply systems is to make certain that each medicine reaching a patient is safe, effective, and of standard quality. QA activities in a hospital or clinic should be comprehensive, spanning the entire supply process from medicine selection to patient use.
To expand your understanding of the determinants of medicine quality. It emphasizes both the technical and managerial actions that can be employed to ensure medicine quality and discusses the role of the Drug and Therapeutics Committee (DTC) in ensuring quality of medicines in the health care system.
Objectives
After completion of this session, participants will be able to—
• Define medicine quality
• Understand how medicine quality is assessed
• Understand how medicine quality is ensured
• Describe the role of the DTC in pharmaceutical quality assurance
Outline
• Key Definitions
• Introduction
• Determinants of Medicine Quality
• How is Quality Assessed?
• How is Quality Assured?
• Important Pharmaceutical Quality Issues for the DTC
• Implications for the DTC
Key Definitions
Pharmaceutical quality assurance—Pharmaceutical quality assurance may be defined as the sum of all activities and responsibilities required to ensure that the medicine that reaches the patient is safe, effective, and acceptable to the patient.
Pharmaceutical quality control—As defined by WHO, quality control is the part of the firm’s process concerned with medicine sampling, specifications, testing, and the organization’s release procedures that ensure that the necessary tests are carried out and that the materials are not released for use, nor products released for sale or supply, until their quality has been judged satisfactory.
Good Manufacturing Practices (GMP)—GMPs are performance standards that WHO and many national governments established for pharmaceutical manufacturers. GMPs are part of the quality assurance activities that ensure that products are consistently produced and controlled to the quality standards appropriate to their intended use and required by drug regulatory authorities. The standards include criteria for personnel, facilities, packaging, quality control, and in most cases, stability testing.
Introduction
The DTC is responsible for evaluation of new medicines before they are added to the formulary. this evaluation must involve efficacy, safety, quality, and cost. This Session will provide information on how to evaluate and manage the quality of medicines being considered for the formulary.
The purpose of a QA program for hospitals and clinics is to ensure that every medicine reaching a patient is safe, effective, and meets quality standards. A comprehensive quality assurance program includes both technical and managerial activities from selection to patient use. Many areas within a health care system may be involved with quality assurance, including procurement, pharmacy, medical, and nursing departments, as well as the DTC.
Ensuring quality of a product is twofold—
• Obtaining quality products that are safe and effective through structured selection and procurement methods
• Maintaining quality products through the appropriate storage, distribution, monitoring and prescribing methods.
A comprehensive program will have the following important characteristics—
• Medicines are selected on the basis of safety and efficacy, in an appropriate dosage form with the longest possible shelf life.
• Suppliers with acceptable quality standards are selected.
• Medicines received from suppliers and donors are monitored to meet quality standards.
• Medicine packaging meets contract quality specifications (e.g., blister packs, kits, bulk container specifications).
• Repackaging activities and dispensing practices maintain quality (e.g., appropriate containers and expiration dates).
• Adequate storage conditions in all pharmaceutical areas are maintained.
• Transportation conditions are adequate (e.g., shipping conditions, temperature exposure).
• Product quality concerns reported by inventory managers, prescribers, dispensers, or patients are addressed and resolved.
Poor-quality medicines may cause a number of serious problems including—
• Lack of therapeutic effect that may lead to prolonged illness or death
• Toxic or adverse reactions
• Waste of limited financial resources
• Diminished program credibility, making the entire health care system less effective and less desirable.
Determinants or Aspects of Medicine Quality
The following characteristics of a medicine determine its quality—
• Identity—The correct active ingredient is present.
• Purity—The medicine is not contaminated with potentially harmful substances.
• Potency—The correct amount of active ingredient is present, usually between 95 and 110 percent of the labeled amount.
• Uniformity—Consistency of, shape, and size of the dosage form do not vary.
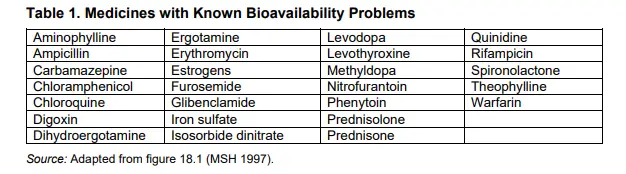
• Bioavailability—Bioavailability refers to the speed and completeness with which an administered medicine enters the blood stream. It must be consistent to provide a predictable therapeutic result. Medicine bioavailability differences exist between manufacturers of the same product. Therefore, careful evaluation of generic medicines
may be necessary before purchase and use. (See table 1.)
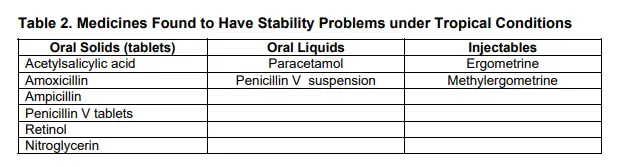
• Stability—The activity of the medicine is ensured for the period of time stated on the product label, that is, until the expiration date. (See table 2.)
• Pharmacopoeial standard—A medicine is of good quality if its characteristics meet the standards described in a widely accepted pharmacopoeia such as the British Pharmacopoeia (BP), European Pharmacopoeia, International Pharmacopoeia (IP), or United States Pharmacopeia (USP).
The lists of medicines in tables 1 and 2 with bioavailability and stability problems represent only a portion of the medicines that may have bioavailability concerns. The U.S. Food and Drug Administration’s “Red Book” (www.fda.gov) lists thousands of products and provides information on bioavailability problems that may exist with some of these medicines. Some examples of bioavailability problems in developing countries include (from Suryawati and Santoso, 1989–95) the following—
• Rifampicin 450 mg capsules. When seven brands of this medicine were studied, researchers found a 100 percent variation in peak concentration between the products suggesting that this medicine has a significant bioavailability problems.
• Captopril. When six brands of this medicine were studied, peak plasma concentrations varied from 75 ng/ml to 275 ng/ml.
• Nifedipine. Peak concentrations varied from 160 ng/ml for a generic medicine to 100 ng/ml for the brand name product.
• Diclofenac slow release tablets. Variable release of the active ingredient and subtherapeutic levels were shown with locally manufactured brands when compared to an imported product.
Critical Elements of a Comprehensive Quality Assurance Program
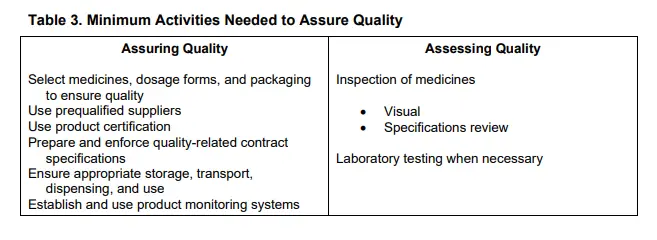
How Is Quality Assessed?
Inspection of Shipments
All shipments of medicines should be quarantined and inspected thoroughly before being released into the supply system. Inspection should include visual inspection and a review of product specifications (including expiration dates) to ensure that the medicine meets specifications.
Laboratory Testing
Medicines should be tested in a laboratory to ensure they meet pharmacopoeial standards. Laboratory testing may not be necessary if reputable suppliers with high quality standards are used when medicines are procured. Pharmacopeial standards can be found in international pharmacopeias such as the British Pharmacopoeia, European Pharmacopoeia, International
Pharmacopoeia, and the United States Pharmacopeia. Medicines that should be tested include—
• Therapeutically critical medicines (cardiovascular and emergency medicines)
• Medicines with known bioavailability or stability problems
• Medicines from new suppliers
• Medicines from suppliers that had quality problems in the past
• Random selection of other medicines to ensure quality.
How Is Quality Assured?
Product Selection
Product selection should be guided by an effective DTC that has thoroughly evaluated the evidence-based information. Preferably, only the dosage forms that have a long shelf-life and are of acceptable stability and bioavailability should be selected.
Selection of Appropriate Suppliers
Suppliers need to be carefully selected and qualified so that only reputable companies will be used to supply pharmaceuticals and medical supplies. To ensure the best suppliers, the following need to be done—
• Have the procurement department establish prequalification and registration of suppliers
• For new suppliers, request samples of intended products before delivery for visual inspection and laboratory analysis
• Request specific reports or data for certain medicines (e.g., bioavailability studies)
• Informally gather information from individuals and companies that have experience with the suppliers .
Product Certification
Obtain appropriate certification of all medicines before accepting for use, including—
• GMP certificate from the drug regulatory authority or from UNICEF Supply Division Warehouse Procurement and Assembly Center (UNIPAC) or other international agency.
• Certificate of pharmaceutical product—WHO-type certificate from the drug control agency of exporting country.
• Batch certification—certificate of batch analysis or assay from manufacturer, drug regulatory agency, or other international quality control organization.
• Random local testing—to confirm quality of the product received.
Contract Specifications
Contract specifications for all medicines should include at a minimum—
• Pharmacopoeia reference standard
• Local language for product label if necessary
• Standards for packaging to meet specific storage and transport conditions.
Appropriate Storage, Transport, Dispensing, and Use Procedures
Policies and procedures need to be in place to ensure the appropriate storage, dispensing, and use of all medicines. These procedures should include at a minimum an explanation of the following—
• Pharmaceutical distribution and control procedures (inventory control and management)
• Provision for appropriate storage and transport
• Cold chain procedures that are enforced explicitly
• Appropriate dispensing and use procedures
{ Containers
{ Labeling
{ Counseling the patient
• Avoidance of repackaging unless appropriate quality control is in place.
Product Monitoring System
The health care system needs a program to monitor the quality of medicines and medical supplies.
Product Problem Reporting System. All quality defects must be reported and the pharmacy or procurement department should keep files of these reports. Procurement, pharmacy, and the DTC should periodically evaluate these reports.
The product problem reporting system should be established at the national or local level that specifies the following—
• Who should report the perceived product quality problem
• How the reporting form is to be filled out
• Where and to whom the reporting form should be sent
What additional measures need to be taken, such as sending samples or information concerning the quantities involved
• What follow-up information will be provided to the person or facility that reported the
problem
• What criteria define when a product will receive further testing or be recalled
• How reports of product problems are filed and retrieved for future procurement needs
Product Recalls. Product recalls will result from two sources:
(a) internally, when a product reporting system identifies unacceptable quality of a product, and
(b) from the manufacturer or drug regulatory agency indicating a product has been identified that no longer meets standards for efficacy, safety, or quality.
The health care system needs a program to identify, retrieve, and return to the supplier any items that have been recalled or that do not meet quality specifications in the health care system.
A national and local program to handle product recalls, should include the following—
• Rapid communication to facilities for quick product recall
• Inventory control systems that track distribution to facilities by batch number
• Recalls classified according to risk to the consumer, such as—
{ No adverse clinical effect
{ Temporary or mild illness
{ Serious illness
{ Death
• Progress of a product recall to ensure complete compliance
Who Ensures Medicine Quality?
Quality of products received in the health care system is the responsibility of many individuals and departments. The procurement department should take the lead role in this endeavor, and the DTC must be an active advisor. The DTC should ensure that all of the departments and individuals listed below are working cohesively to ensure quality products are received.
• Drug Regulatory Authority
ο Registering medicines
ο Inspecting manufacturers for GMP
ο Inspecting pharmacies for compliance with national pharmaceutical policies
ο Sampling and testing medicines as needed
• DTC
ο Selecting medicines for the formulary and procurement
ο Setting technical specifications for pharmaceutical procurement
ο Advising on appropriate storage and transportation of medicines
Coordinating medicine quality testing
ο Reviewing the quality defect reporting system
• Hospital or Clinic Procurement Office
ο Developing specifications for quality
ο Prequalifying suppliers
ο Inspecting products
ο Reporting, tabulating, and taking action on quality defects
• Pharmacy
ο Controlling quality during repackaging
ο Ensuring appropriate storage in the warehouse, pharmacy, and clinics
ο Using appropriate containers for dispensing
ο Instructing patients in appropriate use of medicines
ο Reporting quality defects
• Physicians
ο Monitoring and promoting quality assurance in their facilities
ο Reporting quality defects
• Patients
ο Storing medicines correctly
ο Taking medicines correctly
ο Reporting quality defects
Pharmaceutical Quality Assurance—Implications for the DTC
The DTC is an important component of the hospital or primary care clinic QA program. The DTC should have an active advisory role on all components of the QA program to ensure that medicine are of the highest quality.
The following discussion focuses on areas in which the DTC should be the most involved and may have the most impact. These areas deal with defining product specifications, providing technical advice to the health care organization, and analyzing quality complaints.
Providing Technical Advice on Procurement of Pharmaceuticals
The DTC is responsible for evaluating and selecting medicines for the formulary and the hospital procurement list. Product specifications for procurement should be developed by the DTC and should include medicine name, strength, form, pharmacopoeial standard, bioavailability standard, and expiration dating. This information is best formulated by the DTC (in conjunction with procurement) because this committee has the expertise and experience to provide the technical information that is required.
The DTC is also responsible for providing technical advice on supplier selection, storage of pharmaceuticals and biologicals, transportation methods to ensure quality, and laboratory testing of high-risk products.
Other important considerations procurement issues include the following—
• Procurement of generic medicines
An important function of the DTC is to obtain quality medicines at reasonable prices. The use of multiple-source generic products that are therapeutically equivalent to another product, but less expensive, is an important concept that will help control cost and maintain a high level of quality in medicine selection.
The purchase of generic medicines must provide substitutes that are equivalent in efficacy, safety, and quality.
A therapeutically equivalent product can be defined as a medicine containing the same active ingredient in the same dosage form and of identical strength whose effects with respect to both safety and efficacy are essentially the same. Therapeutic equivalence implies that the product has equivalent bioavailability or is bioequivalent. Generic
medicines that have the same active ingredients may not have the same bioavailability.
• Specifying bioavailability
Bioavailability refers to the speed and the extent of absorption of a medicine’s active ingredient in the blood stream. Bioavailability of generic products may differ between manufacturers of the same product.
Procurement departments must obtain bioavailability data when ordering medicines and must not change manufacturers of a generic product unless bioequivalence of the new product can be assured. Bioavailability data, including laboratory test results, can be obtained from many manufacturers. Any requirements for this data should be included in the tender documents and final contracts with the suppliers. (See table 1 for a list of medicines with known bioavailability problems.)
• Stability of medicines
Stability of a product is of considerable concern and refers to its capacity to maintain potency throughout its shelf life (i.e., until the expiration date). Stability can be ensured,to some degree, by asking for stability studies on products that have known problems and by ensuring that all products are received, stored, and transported at appropriate
conditions, avoiding direct light, temperature extremes, and moisture. Reputable manufacturers will continue to test products throughout the stated shelf life to confirm that the medicine retains its full potency.
Medicines with known stability problems must be handled carefully by the hospital or clinic. These medicines may deteriorate more rapidly than expected, especially in tropical conditions of elevated heat and humidity. Stability testing in the country of purchase may be necessary to ensure that these products indeed have stability throughout the shelf life of the product. (See table 2 for a list of medicines with known stability problems.).
Providing Technical Advice to Other Departments
The DTC should work closely with hospital and clinic departments, including pharmacy,nursing, medical, and supply management staff, to ensure that pharmaceutical quality assurance procedures are practiced throughout the system. All health care personnel should be enlisted and encouraged to participate in a comprehensive QA program to ensure that medicines are procured, stored, administered, dispensed, and used correctly.
Analyzing Product Problem Reports
The DTC should work with drug regulatory agencies, the procurement department, suppliers,pharmacies, physicians, and patients to analyze, evaluate, and take action on quality complaints of products. This function of the DTC is vital to ensure that medicines of good quality are available. Complaints about quality should be analyzed and recommendations developed to deal with quality defects. A medicine recall system must be readily available and effective.
Even the best QA program of a manufacturer, supplier, and a hospital or health clinic may allow a defective product to slip through the system. In addition, many health care professionals and patients will have erroneous perceptions of product quality (e.g., appropriate manufacturers or relationship of price and quality), which makes the requirement for a monitoring system essential.
Activity 1. Quality Assurance Issues and Concerns
List the specific quality assurance concerns in your programs in hospitals and primary care clinics under the following headings—
• Obtaining quality products (source issues): problems with the quality of medicines being supplied by commercial sources, government production, or donors
• Maintaining quality products (supply system issues): problems with quality assurance at the central warehouse, in transit, at local facilities, and the like
• Examples of poor quality: anecdotes illustrating poor quality that do not clearly fit under the above headings
As a part of this exercise, please answer the following questions concerning your quality assurance programs—
1. Are you satisfied with the quality of medicines you receive?
2. Is quality maintained throughout your distribution network?
3. Are there complaints of poor quality by patients or health workers?
4. Is there a formal mechanism for reporting and investigating product quality complaints?
5. What role do you see for the DTC in improving and maintaining quality in your health care system?
6. Does anyone have a particular quality assurance issue with which he or she needs help?
Summary
Quality assurance is the responsibility of many different programs and individuals, including procurement, pharmacy, medical staff, patients, and the DTC. A coordinated effort is required to ensure that all departments work together in dealing with quality assurance. Pharmaceutical quality assurance must have a high priority within the health care system in order for the hospital or clinic to have medicines that are effective, safe, acceptable in quality, and at reasonable cost.
The consequences of poor quality products may lead to ineffective, inappropriate treatment as well as increased cost for the health care system.
A comprehensive quality assurance program should be involved with obtaining quality products and maintaining this quality. Table 3 lists the activities that are needed, at a minimum, to assure that quality products are available to the patient.
ABBREVIATIONS AND ACRONYMS
COA certificate of analysis
DTC Drug and Therapeutics Committee
GMP Good Manufacturing Practices
mcg microgram
mg milligram
ml milliliter
ng nanogram
QA quality assurance
UNICEF United Nations Children’s Fund
UNIPAC UNICEF Supply Division Warehouse Procurement and Assembly Center
VA visual aid
References: Drug and Therapeutics Committee Training Course—Participants’ Guide
This document was made possible through support provided by the U.S. Agency for International Development, under the terms of cooperative agreement number HRN-A-00-00- 00016-00. The opinions expressed herein are those of the author(s) and do not necessarily reflect the views of the U.S. Agency for International Development.
About RPM Plus
RPM Plus works in more than 20 developing and transitional countries to provide technical assistance to strengthen pharmaceutical and health commodity management systems. The program offers technical guidance and assists in strategy development and program implementation both in improving the availability of health commodities—pharmaceuticals,vaccines, supplies, and basic medical equipment—of assured quality for maternal and child
health, HIV/AIDS, infectious diseases, and family planning, and in promoting the appropriate use of health commodities in the public and private sectors.
Recommended Citation
The materials may be freely abstracted, quoted and translated in part or in whole by non-profit or educational organizations (for reference or teaching only) provided the original source is acknowledged. They should not be sold nor used for any other commercial purpose.
Management Sciences for Health and World Health Organization. 2007. Drug and Therapeutics Committee Training Course. Submitted to the U.S. Agency for International Development by the Rational Pharmaceutical Management Plus Program. Arlington, VA: Management Sciences for Health.
Rational Pharmaceutical Management Plus
Center for Pharmaceutical Management
Management Sciences for Health
4301 North Fairfax Drive
Arlington, VA 22203 USA
Phone: 703.524.6575
Fax: 703.524.7898
E-mail: rpmplus@msh.org
Web: www.msh.org/rpmplus
Developed in Collaboration with the
World Health Organization
Geneva, Switzerland